| Description |
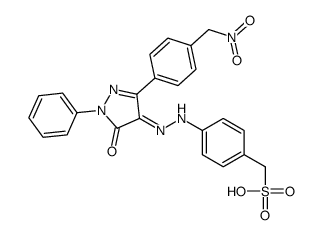
PHPS1 is a potent and selective Shp2 inhibitor with Kis of 0.73, 5.8, 10.7, 5.8, and 0.47 μM for Shp2, Shp2-R362K, Shp1, PTP1B, and PTP1B-Q, respectively[1].
|
| Related Catalog |
|
| Target |
Ki: 0.73 μM (Shp2), 5.8 μM (Shp2-R362K), 10.7 μM (Shp1), 5.8 μM (PTP1B), 0.47 μM (PTP1B-Q)[1]
|
| In Vitro |
PHPS1 (30 μM; 6 days) inhibits proliferation of human tumor cells[1]. PHPS1 (5-20 μM; 5-360 minutes) inhibits Erk1/2 but not Akt and Stat3 phosphorylation in a dose-dependent manner[1]. Cell Viability Assay[1] Cell Line: Human cancer cell lines MDA-MB-435, HCT-116 (colon carcinoma), HCT-15 (colon carcinoma), PC-3 (prostate carcinoma) HT-29 (colon carcinoma), NCI-H661 (lung carcinoma), and Caki-1 (kidney carcinoma) Concentration: 30 μM Incubation Time: 6 days Result: Resulted in a reduction in cell number of between 0% (Caki-1) to 74% (HT-29). Western Blot Analysis[1] Cell Line: Madin-Darby canine kidney (MDCK) cells Concentration: 5, 10, 20 μM Incubation Time: 5, 15, 60, 120, 360 minutes Result: Inhibited HGF/SF (1 unit/mL)-induced phosphorylation and thus activation of Erk1/2 over a time period of 15 min to 6 h. In contrast, transient phosphorylation of Erk1/2 after 5 min was not affected. Exhibited no effect on HGF/SF-induced activation of PI3K/Akt or Stat3.
|
| In Vivo |
PHPS1 (3 mg/kg; i.p. injection; every day during the last week on the high-fat diet) renders Ldlr-/- mice less susceptible to atherosclerosis development[2]. Animal Model: Ldlr-/- (005061) mice[2] Dosage: 3 mg/kg Administration: Intraperitoneal (i.p.) injection; every day during the last week on the high-fat diet. Result: Revealed a significant decrease in atherosclerotic plaque size in the aorta compared with the other two groups.
|
| References |
[1]. Klaus Hellmuth, et al. Specific Inhibitors of the Protein Tyrosine Phosphatase Shp2 Identified by High-Throughput Docking. Proc Natl Acad Sci U S A. 2008 May 20;105(20):7275-80. [2]. Jia Chen, et al. SHP2 Inhibitor PHPS1 Protects Against Atherosclerosis by Inhibiting Smooth Muscle Cell Proliferation. BMC Cardiovasc Disord. 2018 Apr 27;18(1):72.
|