| Description |
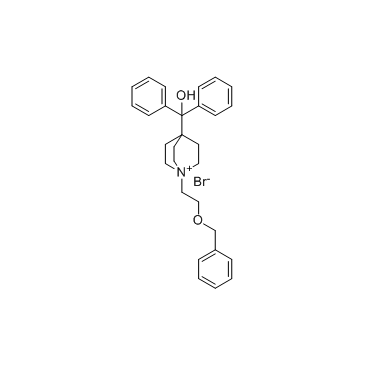
Umeclidinium bromide is a novel mAChR antagonist. The affinity (Ki) of Umeclidinium bromide for the cloned human M1-M5 mAChRs ranges from 0.05 to 0.16 nM.
|
| Related Catalog |
|
| Target |
Ki: 0.16 nM (M1 mAChR), 0.15 nM (M2 mAChR), 0.06 nM (M3 mAChR), 0.05 nM (M4 mAChR), 0.13 nM (M4 mAChR)[1]
|
| In Vitro |
In human embryonic kidney 293 cells, Umeclidinium bromide (GSK573719A) inhibits the human ether-a-go-go-related gene channel tail current in a concentration-dependent manner (IC50=9.4 μM)[1]. Umeclidinium bromide, previously known as GSK573719, is a novel high-affinity specific mAChR antagonist. It is a potent agent that demonstrates slow functional reversibility at cloned human M3 mAChRs and at endogenous mAChR in isolated human bronchus[2].
|
| In Vivo |
When Umeclidinium bromide (GSK573719A) is given once daily to mice for 5 consecutive days (0.025 μg intranasally), the level of inhibition on the fifth day is modestly increased above that obtained after a single administration to the same mice (60 versus 35%, respectively). After the fifth day of dosing, the mice are rested for 5 additional days, allowing bronchomotor tone to return to baseline levels. On the sixth day, the mice receive one last dose of antagonist and are once again challenged with Mch. The level of inhibition is essentially the same as that found on the first day of testing, indicating that tolerance is not evident with repeated intranasal delivery of Umeclidinium bromide. By contrast, when Umeclidinium bromide is given orally (2.0 mg/kg) to mice at a dose 100 times the ED50 value (intranasal), there is no observable protection against an Mch challenge[1].
|
| Kinase Assay |
Ligand binding assays with Umeclidinium bromide (GSK573719A) and [3H]-N-methyl scopolamine (0.5 nM) are performed using a scintillation proximity assay for M1, M2, and M3 mAChRs and a filtration assay for M4 and M5 mAChRs. For the scintillation proximity assay assay, membranes are incubated with wheat germ agglutinin beads in 50 mM HEPES buffer, pH 7.4, at 4°C for 30 minutes and then with the radioligand in a 96-well OptiPlate for 2 hours at room temperature in the presence of vehicle (1% DMSO) or GSK573719 (0.01-300 nM). At the end of the incubation, the plates are centrifuged (for 5 minutes at 2000g), and radioactivity is counted. For the filtration assay, membranes (M4 and M5) are similarly incubated in HEPES buffer containing the radioligand for 2 hours at room temperature in the presence of vehicle (1% DMSO) or Umeclidinium bromide (0.03-300 nM). Atropine is used as a reference agent. Reactions are terminated by rapid filtration through GF/C filters (glass microfiber binder free 1.2 μ). Membranes are washed with ice-cold 50 mM HEPES and transferred to scintillation vials. Radioactivity is counted in a Scintillation Counter. Reactions are terminated by rapid filtration. Data are obtained from three independent experiments. Specific binding is determined by subtracting nonspecific binding (using 0.3 μM atropine) from total binding. The inhibition constant (Ki) for Umeclidinium bromide is calculated. Membranes containing M3 mAChRs are also incubated for 2 hours at room temperature with increasing concentrations of [3H]-N-methyl scopolamine (0.08-9.24 nM) in the presence or absence of Umeclidinium bromide (0.2-0.5 nM) in 50 mM HEPES, pH 7.4. Nonspecific binding is determined using 10 μM atropine. The saturation data are converted to a scatchard plot for analysis[1].
|
| Animal Admin |
Mice[1] Age-matched male BALB/c mice (23-25 gm) are pretreated intranasally (50 μL per mouse) with vehicle (0.9% saline) or Umeclidinium bromide at intervals (0.25-48 hours) prior to methacholine challenge, and placed into individual plethysmograph chambers. Fresh air is supplied by bias flow pumps to the chambers. After baseline respiratory [enhanced pause (Penh)] values are collected, the mice received methacholine (30 mg/mL or EC80) by aerosol delivery (flow=1.6 mL/min×2 minutes). An average Penh is then calculated for 5 minutes. Penh=[(expiratory time/relaxation time)−1]×(peak expiratory flow/peak inspiratory flow), and relaxation time is the amount of time required for 70% of the tidal volume to expire. In some cases, animals are treated on multiple, consecutive days as described in the figure legends. The data are expressed as the mean±S.E.M. percent inhibition of Penh or (mean Penh value of vehicle treated group-Penh for each drug-treated animal) divided by (mean Penh value of vehicle treated group)×100%. Data are analyzed using commercially available software.
|
| References |
[1]. Salmon M, et al. Pharmacological characterization of GSK573719 (umeclidinium): a novel, long-acting, inhaled antagonist of the muscarinic cholinergic receptors for treatment of pulmonary diseases. J Pharmacol Exp Ther. 2013 May;345(2):260-70. [2]. Cazzola M, et al. Pharmacology and therapeutics of bronchodilators. Pharmacol Rev. 2012 Jul;64(3):450-504. [3]. Calzetta L, et al. Pharmacological characterization of the interaction between umeclidinium and vilanterol in human bronchi. Eur J Pharmacol. 2017 Jul 14. pii: S0014-2999(17)30470-3.
|